Research themes in IHES
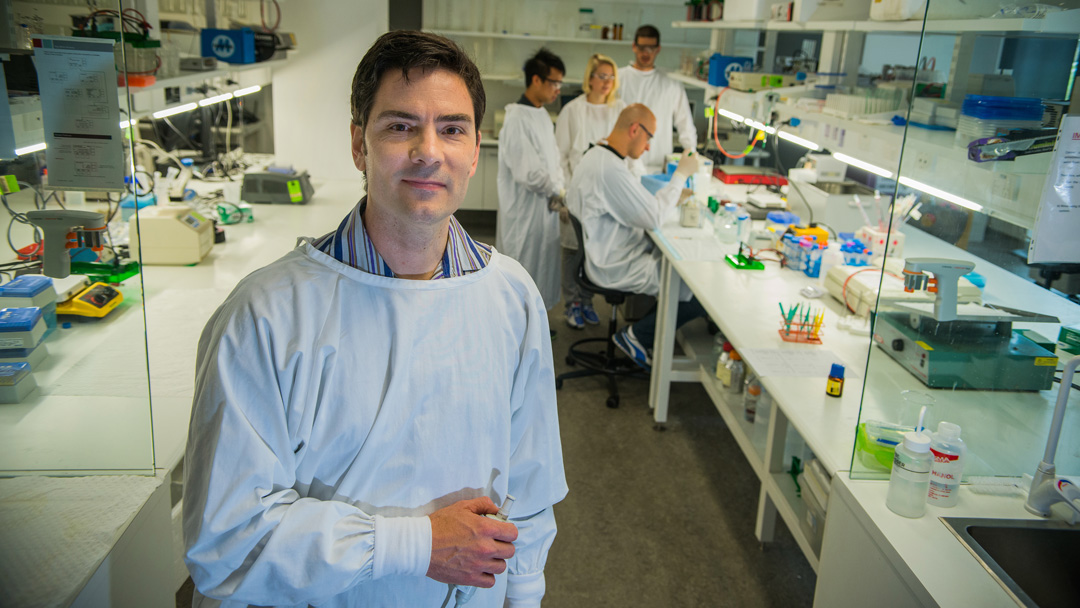
We have three multi-disciplinary research themes which cover healthy futures, sports and movement sciences.
Explore our research themes to learn more about our research and our industry-leading researchers.
Explore our research themes to learn more about our research and our industry-leading researchers.